A bitterly cold night turns critical
Last evening, after my dialysis session, I started the familiar walk toward the station. Andrew was going to meet me on the way to take me home. The night was bitterly cold, and as the chill seeped through my layers, my asthma struck—hard.

I stopped in my tracks, wheezing, and sank onto the fence beside the main road. My breaths were shallow, panic rising with each one. That was when it hit me—I’d forgotten to pack my Ventolin inhaler. Of all nights! After a few moments of rest, I tried again, determined to push through. But within minutes, I was gasping worse than before, my chest tightening like a vice.
Help along the way
Panicking, I called the dialysis unit. Their advice was swift but daunting: “Call an ambulance.” I hung up, took a shaky breath, and dialed 112. The call handler was incredible—calm and steady, guiding me through those frightening moments.
While we waited, Andrew arrived. Seeing me struggling, we decided to move, however slowly, to somewhere warmer. We spotted a nearby Homebase store and shuffled inside. The staff there were angels. They didn’t just help—they went above and beyond. They found a chair for me to sit on and kept watch for the ambulance, even as they locked up the store around us. Their kindness was a lifeline on such a tough night.
Relief in the ambulance
When the ambulance arrived, the crew listened carefully, then moved me inside for a thorough check. After assessing me, they set up a nebulizer with salbutamol, and as I breathed in the soothing mist, relief finally came.
Once stable, the crew drove us to the local Emergency Department. It had been a harrowing night, but thanks to the quick thinking of so many—Andrew, the Homebase staff, the paramedics, and the call handler—I felt deeply grateful to be in good hands.
From asthma to cardiac concerns
The night had been grueling already, but it wasn’t over yet. Once in the Emergency Department, the doctors wanted to run an ECG. At first, I flat-out refused. The thought of those sticky pads on my chest—my sensory nightmare—was unbearable. But Andrew, ever patient, explained why they were so insistent. My blood results had come back, and the doctors were alarmed by elevated troponin levels, a possible indicator of a heart attack.
I was convinced it was an asthma attack—plain and simple. After all, the cold, the panic, the wheezing—it all pointed to that. But for the doctors, cardiac concerns took precedence. They explained that while troponin can rise naturally in dialysis patients, they couldn’t ignore the numbers. Reluctantly, I agreed to the ECG and settled in for what would become a long night of repeated blood tests and consultations.
The long night of tests and waiting
By morning, after hours of waiting and several rounds of tests spaced far apart, the consultants were reasonably confident it wasn’t cardiac. Still, they needed more information. This is where things stalled. The team in Port Laoise tried to access reports from my cardiac investigations over the summer, but the fragmented nature of our health system became an issue. Even by the time I was discharged, it wasn’t clear if those reports had been located.
A fragmented healthcare system
I couldn’t help but feel frustrated. Why, in this digital age, can’t Ireland create a unified online patient record system? One where essential medical information is accessible to any healthcare provider, regardless of location or hospital group? It seems such a simple solution, yet here we are, stuck in silos, wasting precious time.
A long day of waiting
By mid-morning, it seemed like we’d be heading home soon. The doctors gave the impression they were just waiting on a few reports before discharging me. Yet, as the hours dragged on, meaningful communication became nonexistent.
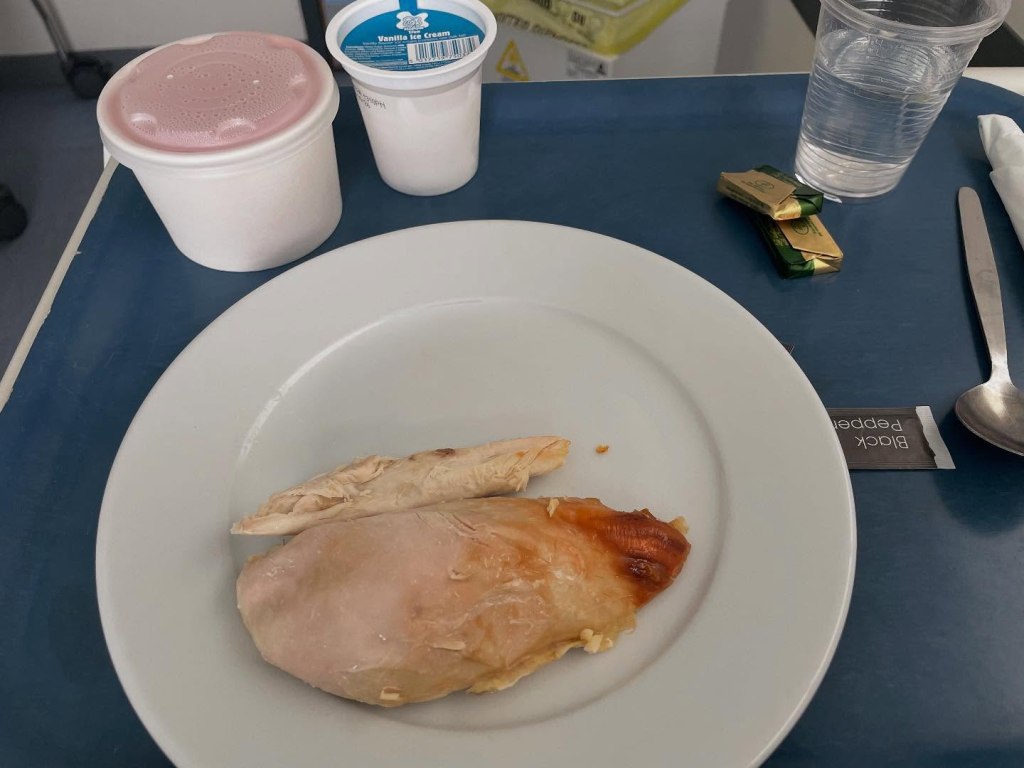
I hadn’t eaten breakfast, so when I was offered a cup of tea, I gratefully accepted it. Lunchtime brought what looked like a lovely meal—chicken, potatoes, and vegetables—but when I asked if it was renal-friendly, it wasn’t. The tray disappeared. A fresh plate of plain chicken was brought instead. There was also the unexpected bonus of jelly and ice cream. The chicken was dry, but hunger made me eat it without complaint.
Still, we waited. Andrew made trips to the vending machine throughout the afternoon, occasionally overhearing snippets of information in the hallway. Inside the room, however, we were kept in the dark.
A duty of care
By 5:30 in the evening, it became clear we couldn’t wait much longer. I had dialysis scheduled for the next day, and Andrew had missed an entire day of his diabetes medication. I was worried about him and knew I had to make sure he was okay, too.
Frustrated, we demanded to see a doctor. Instead, a nurse arrived to check if I had a cannula in my arm. She seemed shocked to find I didn’t. I dislike having a cannula unless absolutely necessary, so I had refused one earlier. Her response was surprising: “Oh, you don’t want a scan, then.”
Confused, we asked, “What scan? No one’s mentioned a scan.”
A race against time
At that moment, the consultant entered the room and finally explained. They wanted a CT scan to rule out a clot in my lungs. If the scan was clear, I could go home. If not, the outcome would be the same, but I’d leave with medication. However, the scan required a cannula.
“Well, put it in, then,” I said without hesitation. “Let’s get on with it.”
The doctor cannulated me, and we waited for a porter to take me to the CT scan. The scan itself was an ordeal; I struggled to stay calm in the machine and nearly had a meltdown. Somehow, I managed to endure it and returned to Andrew.
Answers at last
The results took longer than expected, but they finally arrived. Thankfully, there was no clot in my lungs. However, the scan hinted at a chest infection on the right side. The doctor prescribed a five-day course of antibiotics.
At last, we were allowed to go home. A good friend drove half an hour to pick us up and get us back. Exhausted but relieved, we made it home together, grateful for the support that got us through such a challenging day.
